Understanding brain death can be a complex topic, especially when dealing with medical information in Singapore. It is crucial to process this information correctly to make informed decisions. In this guide, he will break down the concept of brain death and explain how it is determined in medical settings in Singapore. By the end of this blog post, she hopes readers will have a clearer understanding of this important medical topic.
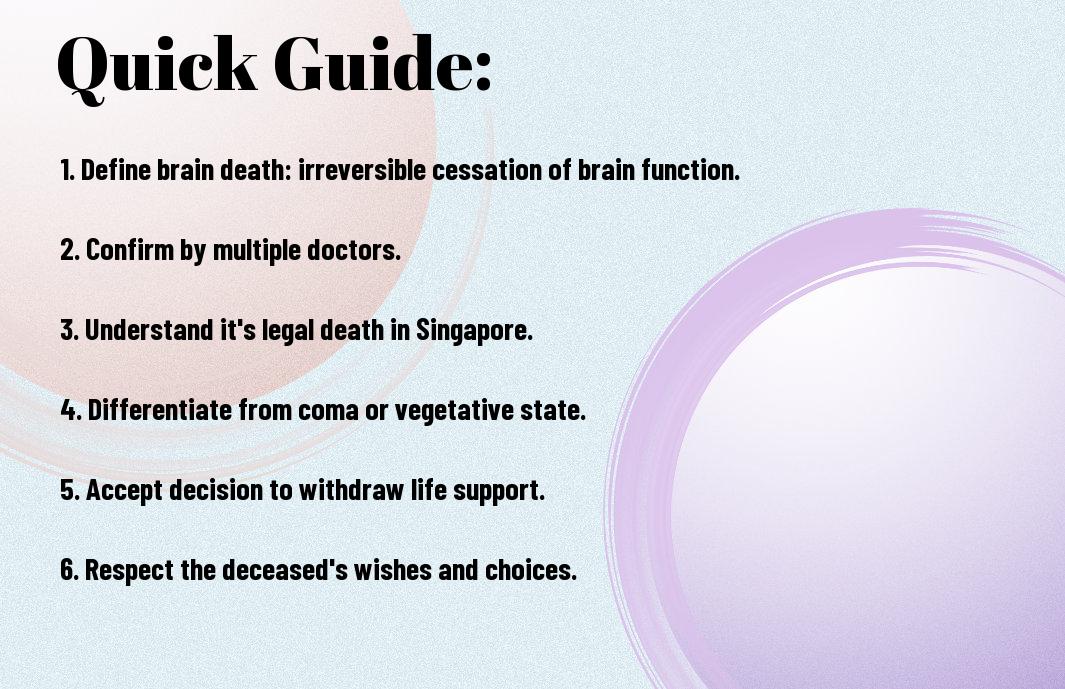
Key Takeaways:
- Brain death is legally recognised as death in Singapore. Once a doctor has determined brain death, it is considered the same as legal death in Singapore.
- Brain death is different from a coma. A coma means the brain is still functioning, while brain death signifies the irreversible loss of all brain function.
- Tests to confirm brain death: A series of tests, including neurological examinations and scans, are conducted to determine brain death accurately.
- Family involvement in decision-making: Family members are usually involved in discussions about brain death and the withdrawal of life-sustaining treatments.
- Organ donation after brain death: Organ donation is possible if a patient is declared brain dead, and it can help save other lives.
Understanding Brain Death
Definition and Diagnosis
Understanding brain death is crucial in the medical field, as it is a complex concept that involves the irreversible loss of all brain functions, including the brainstem. When an individual is diagnosed as brain dead, he or she is considered legally and clinically dead, even though their heart may still be beating with the help of life support machines. The diagnosis of brain death is a meticulous process that involves a series of tests carried out by experienced medical professionals.
Doctors typically look for specific signs to confirm brain death, such as the absence of reflexes, unresponsiveness to pain, and fixed dilated pupils. These indicators, along with other clinical assessments and neuroimaging tests, help in determining the irreversible cessation of all brain functions. It is important to note that brain death is different from a coma or a persistent vegetative state, where some brain functions may still be active.
Family members of a patient diagnosed as brain dead may find it challenging to accept this diagnosis, as the person may appear to be sleeping peacefully due to the assistance of life support machines. However, it is crucial for healthcare providers to explain the diagnosis clearly and provide support to help the family understand the medical reasons behind the determination of brain death.
Medical Criteria for Brain Death
Little room is left for error when determining brain death, as it is crucial to follow strict medical criteria to ensure accurate diagnosis. One common criterion is the absence of any brainstem reflexes, including the gag reflex and pupillary reflex. Additionally, there should be no spontaneous respirations observed, even when the patient is no longer receiving mechanical ventilation.
With advancements in medical technology, neuroimaging tests such as EEGs and cerebral blood flow studies can also be used to confirm the absence of brain activity. These tests provide further evidence to support the clinical findings of brain death, offering a more comprehensive evaluation of the patient’s condition. By combining these medical criteria and tests, healthcare professionals can make a confident diagnosis of brain death.
Types of Brain Death
Clearly, understanding the different types of brain death is crucial in comprehending this complex medical issue. In Singapore, three main types of brain death are recognised: Clinical Brain Death, Brainstem Death, and Whole-Brain Death. Each type has specific criteria that need to be met before a patient can be declared brain dead.
| Clinical Brain Death | Is diagnosed when a person no longer has any neurological function, including the ability to breathe on their own. |
| Brainstem Death | It occurs when the patient has lost all brainstem functions, such as the ability to maintain their own heartbeat and breathing. |
| Whole-Brain Death | It is declared when there is a total and irreversible loss of all brain function, including the brainstem. |
Clinical Brain Death
With Clinical Brain Death, a patient is determined to be brain dead based on the absence of neurological function. This means that he or she no longer has the capacity to breathe independently and there is no activity in the brain.
When diagnosing Clinical Brain Death, doctors perform a series of specific tests to confirm the lack of brain function, such as assessing responses to stimuli and checking for brain activity using imaging techniques.
Assume that if a person is diagnosed with Clinical Brain Death, it means that he or she is considered legally and medically dead, even though the heart may still be beating with the help of life support.
Brainstem Death
Some patients experience Brainstem Death, where there is a complete loss of all brainstem functions. This includes crucial involuntary actions such as regulating breathing, heartbeat, and blood pressure.
Brianstem Death is often diagnosed through specialised tests that observe the absence of brainstem reflexes, such as the gag reflex and the pupillary reflex, indicating a severe and irreversible loss of brain function.
To determine brain stem death, doctors need to ensure that there is no chance of recovery and that the condition is irreversible before making the diagnosis.
Whole-Brain Death
Death is declared whole-brain death when a person has suffered an irreversible loss of all brain functions, including higher brain functions and the brainstem. This signifies a complete cessation of all brain activity.
Whole-Brain Death is determined through a series of rigorous neurological examinations, including tests to assess responsiveness, cranial nerve functions, and brain activity. Once these criteria are met, the patient can be declared legally dead.
Assume that when a patient is diagnosed with Whole-Brain Death, there is no chance of recovery or survival, and the focus shifts to providing compassionate end-of-life care.
Factors Contributing to Brain Death
-
Unlike other forms of death, brain death is a complex process that involves various factors. It is imperative to understand the different causes that can lead to brain death.
Traumatic Brain Injury
With traumatic brain injury being one of the leading causes of brain death, it is crucial to recognise the severity of head injuries. In cases of severe trauma, such as a serious car accident or a fall from a significant height, the brain can suffer irreversible damage. This damage can lead to cessation of brain function, ultimately resulting in brain death.
In some cases, even with immediate medical intervention, the extent of the injury may be too severe to recover from. The brain’s ability to regulate imperative functions like breathing and heart rate can be compromised, leading to irreversible brain damage.
Recognising the signs of a traumatic brain injury and seeking prompt medical attention can be critical in preventing brain death in such cases.
Stroke and Cerebrovascular Accidents
While stroke and cerebrovascular accidents are another significant cause of brain death, they occur due to the interruption of blood flow to the brain. When a stroke deprives the brain of oxygen for an extended period of time, brain cells begin to die rapidly, leading to irreversible damage.
In these cases, the brain’s ability to function and sustain vital processes is severely compromised. Without adequate blood flow and oxygen supply, the brain cannot survive, eventually resulting in brain death. Early recognition of stroke symptoms and timely medical intervention are crucial in preventing irreversible brain damage.
Factors such as high blood pressure, diabetes, and smoking can increase the risk of strokes, highlighting the importance of managing underlying health conditions to prevent brain death due to cerebrovascular accidents.
Infections and Inflammatory Diseases
Some infections and inflammatory diseases can also contribute to brain death. Conditions such as meningitis or encephalitis can cause inflammation of the brain, leading to severe damage and impairment of brain function.
In these cases, the body’s immune response can inadvertently attack the brain tissues, causing irreversible harm. If not promptly diagnosed and treated, these conditions can progress rapidly, ultimately resulting in brain death.
This highlights the importance of early detection and appropriate treatment of infections and inflammatory diseases to prevent the progression to brain death.
Processing Medical Information in Singapore
Overview of Singapore’s Healthcare System
After a diagnosis, understanding the medical information provided is crucial for making informed decisions. In Singapore, the healthcare system is widely recognised for its efficiency and high standards. The system is a blend of public and private healthcare providers, offering a range of services from primary care to specialised treatments.
Singapore boasts a universal healthcare system where the government plays a significant role in ensuring access to affordable and quality healthcare for all residents. Patients in Singapore have the flexibility to choose between public institutions like polyclinics and hospitals or private medical practices and hospitals for their healthcare needs.
With a focus on preventive care and health education, Singapore’s healthcare system also encourages individuals to take responsibility for their own health and well-being. This proactive approach helps in early detection and management of health conditions, ultimately leading to better healthcare outcomes.
Role of Doctors and Medical Professionals
Systematically processing medical information in Singapore involves understanding the crucial role that doctors and medical professionals play in the provision of healthcare. Doctors in Singapore undergo rigorous training and are held to high professional standards to ensure the delivery of quality care to patients.
Medical professionals in Singapore work collaboratively in multidisciplinary teams to provide holistic care and tailor treatment plans to individual patient needs. This approach ensures that patients receive comprehensive and personalised healthcare services, promoting better health outcomes and patient satisfaction.
Doctors and medical professionals in Singapore also participate in ongoing professional development to stay abreast of the latest advancements in medical science and technology. This commitment to continuous learning and improvement enhances the quality of healthcare delivery in the country.
Patient Rights and Responsibilities
Medical information processing in Singapore also involves understanding patient rights and responsibilities within the healthcare system. Patients have the right to access their medical records, make informed decisions about their care, and seek second opinions if needed. It is important for patients to be actively involved in their healthcare journey, asking questions and seeking clarification when necessary.
Doctors in Singapore are required to respect patient confidentiality, provide clear and accurate information about diagnoses and treatment options, and involve patients in decision-making processes regarding their care. This patient-centred approach fosters trust and mutual respect between healthcare providers and patients, leading to better health outcomes.
Responsibilities such as adhering to prescribed treatment plans, following medical advice, and keeping appointments are vital for patients in Singapore to ensure effective healthcare delivery and optimal health outcomes. By actively participating in their care and taking ownership of their health, patients can contribute to a positive healthcare experience for themselves and those involved in their treatment.
Step-by-Step Guide to Understanding Brain Death Diagnosis
For a clear understanding of how brain death diagnosis is conducted, the process can be broken down into key steps. The table below outlines these steps in a simple and organised manner:
| Step | Description |
| Initial Assessment and Examination | First evaluation of the patient’s neurological status. |
| Imaging Tests and Scans | Performing imaging studies to assess brain function and blood flow. |
| Confirmatory Tests and Procedures | Carrying out specific tests to confirm irreversible loss of brain function. |
Initial Assessment and Examination
examination begins with a thorough assessment of the patient’s neurological function, including tests for reflexes, responsiveness, and cranial nerve function. The healthcare team will evaluate the patient’s pupils for responses to light, check for any signs of spontaneous movement, and assess the patient’s ability to breathe on their own.
Following the initial assessment, specialised neurological tests may be conducted to further evaluate brain function. These tests can include assessing the patient’s response to pain stimuli, determining if there is any brainstem activity present, and conducting an apnea test to confirm the absence of respiratory drive.
In cases where the initial assessment suggests possible brain death, further confirmatory tests will be carried out to declare brain death formally. These tests are important to ensure accuracy in diagnosis and typically involve a multidisciplinary team of healthcare professionals.
Imaging Tests and Scans
With imaging tests such as CT scans, MRI scans, or cerebral angiography, healthcare providers can visualise the brain’s structure and blood flow patterns. These scans help identify any structural abnormalities, such as bleeding or swelling, that may be contributing to the patient’s condition.
Imaging tests play a crucial role in ruling out any potentially reversible causes of coma or unresponsiveness. They provide valuable information to the medical team so they can make an informed decision regarding the patient’s prognosis and the presence of irreversible brain damage.
Assessment of brain activity through imaging tests also helps in determining the extent of brain injury and assists in establishing a timeline of events leading to brain death. This detailed information is vital for healthcare providers to make accurate and ethical decisions regarding patient care.
Confirmatory Tests and Procedures
Assuming initial assessments and imaging tests suggest brain death, confirmatory tests such as an electroencephalogram (EEG) or cerebral blood flow studies may be conducted. These tests are crucial in providing objective evidence of complete and irreversible loss of brain function.
Brain death confirmation is a meticulous process that follows set protocols and guidelines to ensure accuracy. To eliminate any chance of error in the diagnosis of brain death, various healthcare professionals conduct numerous assessments and tests. Once brain death is confirmed, the patient is considered legally and clinically dead.
Tips for Family Members and Carers
Your loved one’s medical condition can be overwhelming, but there are ways to navigate through this challenging time. Here are some tips to help you provide the best care and support:
- Keep up with the medical information that the healthcare team is providing.
- Ask questions to clarify any doubts or uncertainties you may have.
- Seek emotional support from friends, family, or support groups.
Assume that the healthcare team has your loved one’s best interests at heart and trust their expertise in managing the situation.
Coping with the Diagnosis
Any diagnosis of brain death is difficult to process. It is normal to feel a range of emotions, including shock, disbelief, anger, and sadness. Family members and carers may experience feelings of helplessness and confusion. Seeking support from each other and mental health professionals can help in coping with these emotions.
It is crucial to communicate openly and honestly with the medical team to understand the diagnosis and prognosis clearly. They can provide guidance on how to navigate through this challenging time and make decisions in the best interest of the patient.
Family members and carers may also benefit from seeking counselling or therapy to help them process their emotions and gain a better understanding of the situation. It is crucial to take care of one’s mental and emotional well-being while supporting their loved one through this difficult time.
Making Informed Decisions
Family members play a crucial role in making decisions regarding the care and treatment of a patient with brain death. Any decisions regarding life support, organ donation, or end-of-life care should be well-informed and made in consultation with the healthcare team. It is important to consider the patient’s wishes, values, and beliefs when making these decisions.
With clear communication and information provided by the healthcare team, family members and carers can feel more empowered to make decisions that align with the patient’s best interests. Making informed decisions can help ensure that the patient receives the appropriate care and treatment according to their wishes.
Supporting the Patient
diagnosis of brain death can be distressing for both the patient and their loved ones. It is crucial to provide emotional support and comfort to the patient during this difficult time. Family members and carers can help create a peaceful and supportive environment for the patient by being present, offering words of encouragement, and maintaining a sense of normalcy.
It is important to respect the dignity and autonomy of the patient throughout the process. Providing emotional support can help alleviate any feelings of fear or loneliness the patient may be experiencing. Family members and carers can also work closely with the healthcare team to ensure that the patient’s physical and emotional needs are met.
It is crucial to be patient and understanding while supporting the patient through this challenging time. Showing empathy and compassion can make a significant difference in how the patient and their loved ones cope with the diagnosis of brain death.
Understanding Organ Donation and Transplantation
The Process of Organ Donation
Many people in Singapore may not fully understand the process of organ donation. When a person is declared brain dead, their organs can be donated to save the lives of others in need. This process involves a medical team carefully assessing the viability of the organs for donation, matching them with suitable recipients, and performing the necessary surgical procedures to retrieve and transplant the organs. Organ donation is a selfless act that can have a profound impact on the lives of those in need of organ transplants. It is important for individuals to discuss their wishes regarding organ donation with their loved ones and healthcare providers to ensure that their wishes are respected in the event of brain death. By being informed about the process of organ donation, individuals can make a positive contribution to society even after they have passed away.
Types of Organs That Can Be Donated
Organ donation can involve various types of organs that are critical for the survival and well-being of recipients. These organs include the heart, lungs, liver, kidneys, and pancreas. Each of these organs plays a vital role in maintaining the functions of the body, and their transplantation can significantly improve the quality of life for those in need.
- Heart
- Lungs
- Liver
- Kidneys
- Pancreas
Any individual can choose to donate their organs upon their death, regardless of age or medical history. It is necessary to raise awareness about the importance of organ donation and encourage more people to consider registering as organ donors to help save lives.
Benefits of Organ Donation
Little is known about the benefits of organ donation for both donors and recipients. Donating organs can bring a sense of fulfilment and purpose to individuals, knowing that they have made a significant contribution to the well-being of others. For recipients, organ transplantation can be a life-saving procedure that improves their health and quality of life. Organ donation also promotes a sense of community and unity among individuals, fostering a culture of compassion and altruism. By understanding the benefits of organ donation, individuals can make informed decisions about becoming organ donors and potentially transform the lives of those in need.
To further enhance understanding of the benefits of organ donation, it is crucial to educate the public about the positive impact of this selfless act on individuals, families, and society as a whole.

Pros and Cons of Organ Donation
Now, the pros and cons of organ donation are important aspects to consider when making an informed decision about this altruistic act.
Advantages of Organ Donation
One of the main advantages of organ donation is the opportunity to save lives. By donating organs such as the heart, liver, kidneys, lungs, and pancreas, one person can potentially save or improve the lives of up to eight individuals. This act of generosity can have a profound impact on recipients and their families, giving them a second chance at life.
Organ donation also promotes a sense of community and altruism. By choosing to donate organs, one is contributing to the greater good and helping those in need. This selfless act can inspire others to consider organ donation and create a culture of giving that benefits society as a whole.
Furthermore, organ donation can provide comfort and solace to the donor’s family. Knowing that their loved one’s organs have helped others in need can bring a sense of pride and peace during a difficult time of loss and grief.
Disadvantages and Concerns
Clearly, there are concerns and disadvantages associated with organ donation that one must carefully consider. Some individuals may have religious or cultural beliefs that conflict with the idea of organ donation, leading to ethical dilemmas and personal conflicts. Additionally, there may be fears about the medical process of organ donation and concerns about the impact on the donor’s body post-donation.
Consent issues and respect for the donor’s wishes are also important factors to consider. Without clear communication and understanding of the donor’s intentions, disputes and ethical dilemmas can arise among family members and medical professionals. It is crucial to address these concerns and ensure that the donor’s wishes are respected and followed.
Moreover, there are risks of complications and medical errors associated with organ donation procedures. While advancements in medical technology have reduced these risks significantly, there is still a chance of complications during the donation process that could impact the donor’s health and well-being.
Addressing Common Misconceptions
Donation
One common misconception about organ donation is the myth that doctors may not try as hard to save a registered organ donor’s life in an emergency situation. This is simply not true: healthcare professionals are dedicated to saving lives and will do everything in their power to provide the best possible care to all patients, regardless of their organ donor status.
Another misconception is the belief that organ donation is only for young and healthy individuals. In reality, organs from older donors or those with certain medical conditions can still be viable for transplantation and can save lives. It is important to dispel these myths and educate the public about the inclusivity and impact of organ donation.
Addressing misconceptions and increasing awareness about organ donation can help debunk myths and encourage more individuals to consider becoming organ donors. By providing accurate information and fostering open discussions, society can work towards increasing the number of organ donors and saving more lives in need.
Factors Affecting Organ Donation Rates
Many factors can influence organ donation rates in any country, including Singapore. These factors range from cultural and religious beliefs to education and awareness, as well as healthcare infrastructure and resources. Understanding these factors is crucial in developing strategies to increase organ donation rates and save more lives.
Cultural and Religious Beliefs
While Singapore is a multi-cultural society, cultural and religious beliefs play a significant role in determining attitudes towards organ donation. Some communities may have reservations about organ donation due to religious practices or cultural taboos. It is important to respect these beliefs and educate individuals on how organ donation can align with their cultural values. Providing accurate information and dispelling myths can help address misconceptions and increase acceptance of organ donation within diverse communities.
Education and Awareness
Factors such as education and awareness also play a vital role in influencing organ donation rates. Public campaigns, school programmes, and community outreach can help raise awareness about the importance of organ donation. Education sessions that explain the organ donation process, the impact it can have on saving lives, and how individuals can register as donors are important in encouraging people to make informed decisions about organ donation. Increased awareness and understanding of organ donation among the general public can have a positive impact on donation rates. By empowering individuals with accurate information and highlighting success stories of organ recipients, more people may be inclined to support and participate in organ donation initiatives. After all, education is key in breaking down barriers and misconceptions surrounding organ donation.
Healthcare Infrastructure and Resources
For a country like Singapore to effectively support organ donation, a robust healthcare infrastructure and sufficient resources are important. Having trained medical professionals, proper facilities for organ retrieval and transplantation, and streamlined processes for organ donation can significantly impact donation rates. Moreover, investing in research and technology to improve transplant outcomes and increase the availability of organs is vital in addressing the growing demand for organ transplants. A well-functioning healthcare system that prioritises organ donation can lead to higher donation rates and better outcomes for both donors and recipients. By ensuring that the infrastructure and resources are in place to support organ donation efforts, Singapore can continue to make progress in saving lives through organ transplantation.
Step-by-Step Guide to Organ Donation
All information should be presented in a clear and concise manner to help individuals understand the process of organ donation in Singapore. The following table provides a step-by-step guide to organ donation:
| Step | Description |
| 1 | Register to become an organ donor |
| 2 | Inform family members of your decision |
| 3 | Ensure your donor card is easily accessible |
| 4 | Medical assessment to determine organ suitability |
| 5 | Organ retrieval and transplantation process |
Registering to Become an Organ Donor
Guide individuals interested in becoming organ donors to register their decision with the relevant authorities. This process usually involves signing up on the National Organ Transplant Unit’s website or visiting a nearby healthcare facility to complete the necessary forms. Once registered, the individual will receive a donor card to indicate their consent for organ donation. It is important to inform family members of this decision to ensure they are aware of the individual’s wishes.
The Donation Process
Donors should be aware of the organ donation process, which includes a medical assessment to determine the suitability of organs for transplantation. This assessment involves evaluating the donor’s medical history, performing tests to assess organ function, and ensuring that the organs are healthy for transplantation. Following the discovery of a suitable match, the organ retrieval procedure and organ transplantation into needy recipients take place. It is a carefully orchestrated process that requires coordination between healthcare professionals and transplant teams.
Donors play a crucial role in saving lives through the donation of organs. By making the decision to become an organ donor, individuals can make a significant impact on the lives of those awaiting transplants. It is a selfless act that can provide hope and a new lease on life for recipients. Registering as an organ donor is a powerful way to leave a lasting legacy and make a difference in the lives of others.
Support for Donor Families
Little support is available for the families of donors who have generously given the gift of life through organ donation. During this emotional time, families may require assistance and counselling to cope with the loss of their loved one. Support organisations such as the National Organ Transplant Unit provide guidance and emotional support to donor families throughout the donation process and beyond. They offer resources to help families understand the impact of organ donation and navigate the grieving process.
Donor families play a crucial role in the organ donation process and are often referred to as the “unsung heroes” of transplantation. Their decision to honour their loved one’s wishes and donate organs can bring comfort and healing to both the donor’s family and the recipients of the organs. It is vital to acknowledge and support donor families during this challenging time as they navigate their emotions and find solace in knowing that their loved one’s legacy lives on through organ donation.
Tips for Healthcare Professionals
For healthcare professionals working in the field of brain death, it is crucial to approach their role with sensitivity and empathy. Patients and families are often dealing with highly emotional and distressing situations, and clear communication can make a significant difference in their experience.
- Clearly explain medical terminology and procedures in simple language.
- Listen actively to patients and families, allowing them to express their concerns and fears.
- Provide support and resources for counselling or further information as needed.
The ability to communicate effectively with patients and families is vital in providing quality end-of-life care. When discussing sensitive topics such as brain death, it is important for healthcare professionals to be compassionate and understanding in their approach.
Communicating with Patients and Families
Clearly communicating the diagnosis of brain death to patients and families is a challenging task that requires compassion and empathy. Healthcare professionals should provide information in a clear and understandable manner, allowing time for questions and emotional processing.
Supporting families through the difficult decision-making process that may follow a brain-death diagnosis is a crucial aspect of end-of-life care. Offering guidance on treatment options and respect for the patient’s wishes can help families navigate this challenging time with more clarity and understanding.
It is important for healthcare professionals to be patient and empathetic when communicating with patients and families about end-of-life care. By providing clear information and emotional support, they can help alleviate some of the stress and confusion that often accompany these difficult situations.
Managing End-of-Life Care
Some healthcare professionals may find it challenging to navigate the complexities of end-of-life care, especially in cases of brain death. It is vital to prioritise the comfort and dignity of the patient while also supporting their loved ones through the grieving process.
The management of end-of-life care requires a multidisciplinary approach, involving not only medical expertise but also emotional support and ethical considerations. By collaborating with colleagues from various disciplines, healthcare professionals can ensure a holistic approach to care that addresses all aspects of the patient’s well-being.
Ensuring that the patient’s wishes and values are respected throughout the end-of-life care process is a fundamental aspect of ethical practice for healthcare professionals. By upholding principles of autonomy and beneficence, they can provide care that is not only medically appropriate but also aligned with the patient’s values and preferences.
Ensuring Ethical Practice
The ethical practice of healthcare professionals in managing brain death cases involves upholding the principles of beneficence, non-maleficence, and respect for patient autonomy. It is vital to consider the ethical implications of every decision made in the care of a patient with brain death.
Common Misconceptions about Brain Death
Debunking Myths and Misunderstandings
To debunk myths and misunderstandings surrounding brain death, it is important to provide clear and accurate information. One common misconception is that a patient in a brain-dead state has a chance of recovery. However, brain death is irreversible, and there is no chance of waking up or resuming normal brain function. Another myth is that the individual’s heart is still beating in a brain-dead state. In reality, any movement observed is due to life support equipment.
Furthermore, some may mistakenly believe that brain death is the same as a coma. While coma patients have some brain activity, brain-dead individuals have no brain function at all. Understanding these distinctions is crucial in dispelling misconceptions and promoting accurate knowledge about brain death.
Educating the public, healthcare professionals, and policymakers about the precise criteria and science behind brain death is vital in addressing these myths and misunderstandings. By promoting awareness and clarity on this complex medical phenomenon, society can better understand and accept the realities of brain death.
Addressing Fears and Concerns
If individuals have fears or concerns about brain death, it is important to seek information from healthcare providers or support groups. Often, the fear of the unknown can lead to misconceptions and anxiety. By openly discussing these concerns with knowledgeable professionals, one can gain a clearer understanding of what brain death entails and how it differs from other medical conditions.
Addressing fears and concerns also involves highlighting the compassionate aspect of organ donation. Understanding that organ donation after brain death can save lives and provide hope to those in need may help alleviate fears and misconceptions. Providing support and information to individuals navigating these difficult decisions is crucial in promoting a more informed and compassionate society.
Promoting Public Education and Awareness
Death is a sensitive and complex topic, but promoting public education and awareness about brain death can help demystify the process. By engaging in open conversations, sharing accurate information through various channels, and providing opportunities for questions and discussions, society can become more informed and accepting of brain death as a medical reality.
Plus, increasing awareness about the importance of organ donation and the difference it can make in saving lives is a crucial aspect of public education. By focusing on the positive outcomes and the impact of organ donation, misconceptions and fears surrounding brain death can be gradually replaced with understanding and support for donation initiatives.
Resources for Further Learning
Online Resources and Websites
Not all information about brain death can be found in one place, so it is crucial to explore various online resources and websites to gain a comprehensive understanding. While there are reputable websites such as the Singapore Ministry of Health and medical institutions like Tan Tock Seng Hospital that provide detailed information on brain death, international platforms like the World Health Organisation (WHO) website can also offer valuable insights. Additionally, online forums and discussion boards can be beneficial for individuals to share personal experiences and exchange information.
When accessing online resources, it is important to critically evaluate the credibility of the sources and cross-reference information to ensure accuracy. Furthermore, staying updated with the latest research and guidelines on brain death is crucial for anyone seeking in-depth knowledge on the subject.
Interactive platforms, like webinars and online courses, can also be valuable tools for learning more about brain death. They provide an opportunity for individuals to engage with experts in the field and ask specific questions to enhance their understanding.
Books and Academic Journals
Online resources may provide a wealth of information, but delving into books and academic journals can offer a more detailed and nuanced perspective on brain death. Online, there are books like “The Definition of Death: Contemporary Controversies” by Stuart J. Youngner and “Brain Death” by Eelco F.M. Wijdicks that provide comprehensive insights into the medical, ethical, and legal aspects of brain death.
Academic journals such as the Singapore Medical Journal and the Journal of Critical Care can also be valuable sources for in-depth research articles and case studies related to brain death. These publications are peer-reviewed and offer authoritative information for individuals looking to expand their knowledge in the field.
Plus, exploring academic databases like PubMed and Google Scholar can lead to a plethora of research papers and studies on brain death, providing a deeper understanding of the topic from scientific and medical perspectives.
Support Groups and organisations
Support groups and organisations dedicated to discussing brain death and related issues can be valuable resources for individuals seeking emotional support and practical guidance. On a local level, organisations like the Brain Death Support Group in Singapore can provide a platform for individuals to share their experiences, connect with others facing similar situations, and access resources on coping with the complexities of brain death.
Engaging with support groups can help individuals navigate the emotional and ethical challenges that may arise when dealing with brain death in a loved one. These groups often offer counselling services, educational materials, and opportunities to participate in advocacy efforts to raise awareness about brain death in the community.
Support from these groups can play a significant role in helping individuals cope with the emotional strain of decision-making processes surrounding brain death and provide a sense of community and understanding during difficult times.
To wrap up,
Understanding Brain Death: A Simple Guide To Processing Medical Information In Singapore has provided valuable insights into a complex medical topic. By breaking down the definition of brain death, explaining the criteria for diagnosis, and outlining the legal implications in Singapore, readers can now navigate this sensitive subject with more clarity.
Having a basic understanding of brain death is crucial for making informed decisions regarding medical treatment, organ donation, and end-of-life care. By demystifying this concept, individuals can advocate for themselves or their loved ones with confidence when faced with such challenging situations.
Ultimately, being equipped with accurate information about brain death empowers individuals to engage in meaningful discussions with healthcare professionals, ensuring that end-of-life decisions are made in alignment with personal values and beliefs. This guide serves as a foundation for further exploration and discussions on this important aspect of medical ethics and healthcare in Singapore.
FAQ
Q: What is brain death?
Brain death is the total and irreversible loss of all brain function, including the brainstem. It is the legal and medical definition of death in Singapore.
Q: How is brain death diagnosed?
A: Qualified medical professionals, typically neurologists or neurosurgeons, conduct a series of neurological tests to identify brain death. These tests assess if there is any brain function present.
Q: Can a person recover from brain death?
A: No, brain death is irreversible. Once a person is declared brain dead, there is no chance of recovery, as there is a complete and permanent loss of all brain function.
Q: What are the ethical considerations surrounding brain death?
Ethical considerations include respecting the wishes of the individual regarding organ donation, ensuring a proper and accurate diagnosis of brain death, and providing support to the family during this difficult time.
Q: How is organ donation related to brain death?
Organ donation is often possible in cases of brain death, as the vital organs can be kept functioning for a short period after brain death is diagnosed. This allows for the possibility of donating organs to save other lives.





